What Is IVF Treatment ?
In Vitro Fertilization, commonly referred to as IVF, is a procedure in which extracted eggs from the woman’s ovaries fertilised with sperm samples in a laboratory. If the eggs fertilized, one or two healthy embryos (fertilised eggs) are are transferred into the woman’s uterus. After that if an embryo implants itself in the uterine wall, the woman becomes pregnant. Remaining healthy embryos can be frozen for storage.
Through our partnership with IVF clinics we are pleased to provide immediate access to infertility treatment at affordable prices. Patients can rest assured that we will collaborate and explore all treatment options, providing the best care available.
Couples with both female and male factor infertility may benefit from IVF treatment. IVF increase the chance of pregnancy for woman who are suffering from tubal disease, endometriosis, failure of ovulation, male factor infertility and unexplained infertility.
IVF may be necessary for infertility issues such as,
- Tubal disease; blocked or damaged fallopian tubes
- Reduced ovarian function
- Polycystic ovary syndrome
- Endometriosis
- Uterine fibroids
- Male infertility; reduced sperm count or abnormalities in sperm
- Unexplained infertility
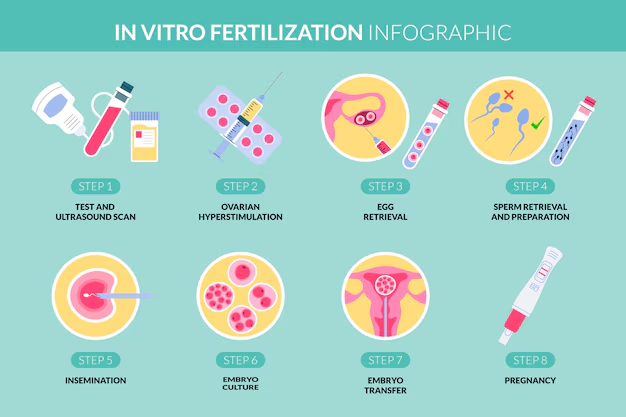
IVF consists of five steps for completion of one IVF cycle.
STEP 1: Overian stimulation:
In a normal menstrual cycle, women ovulate one egg. With the use of various medications to stimulate multiple eggs in the ovaries amount of follicles can be increased. When the eggs reach the proper size, patient receives a hCG injection Eggs are retrieved after 36 hours.
STEP 2: Egg retrieval
When the follicles are determined mature the patient’s eggs are retrieved under anesthesia by using ultrasound guidance, and sent to the laboratory for fertilization. The egg retrieval process (Transvaginal Aspiration) usually takes 30 minutes and the patient is able to go home after a few hours later.
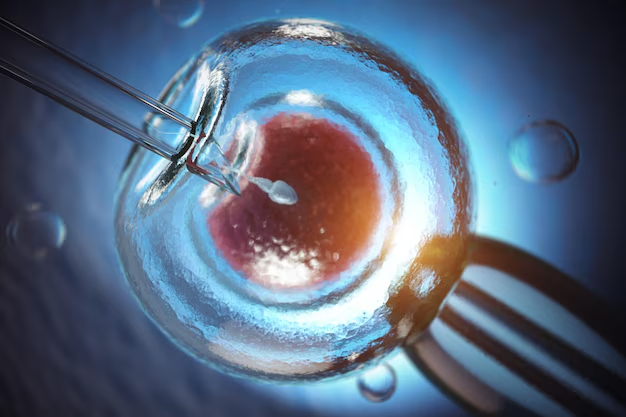
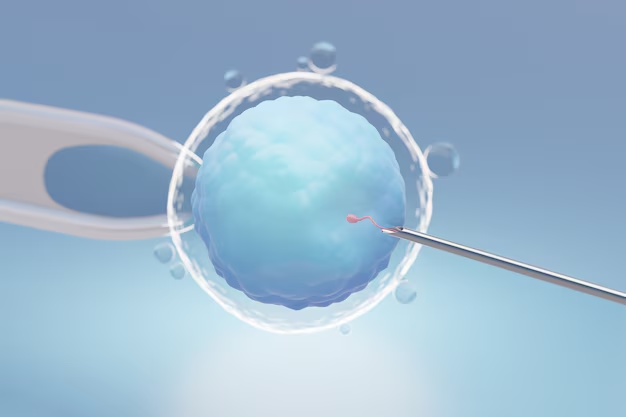
STEP 3: Insemination (Fertilization)
The fertilization process involves placing healthy sperms with each egg and left to incubate overnight. In some cases when achieving fertilization is difficult, a single sperm is injected into each egg. This process is called ICSI (injecting the sperm into the egg). Fertilization occurs after 16 hours.
STEP 4: Embryo culture
2 days after fertilization,eggs become 2 to 4 cell embryos. 5 days after fertilization the embryos are developed and become blastocysts. After that blastocysts and emryos are graded according to the number of cells, symmetry of growth and degree of fragmentation. If needed PGD/PGS can be performed to blastocysts.
STEP 5: Embryo Transfer
Generally 5-6 days after after fertilization, embryos are placed into the most favorable part of the uterus. The number of embryos transferred depends on the patient’s health status, age and the embryo quality. Remaining embryos can be frozen and stored for future cycles by cryopreservation. After two weeks blood pregnancy test is performed.
What Is Oocyte Freezing?
When a baby girl is born, she is born with an egg reserve that contains a certain number of Oocytes (eggs). When a female reaches a certain age and puberty she her menstrual cycle will begin, and she will ovulate and release an egg each month. The rate of which the egg reserve decreases is due to genetic factor and or environmental factors effecting the female. So menopause is reached when the egg reserve has finished and the ovaries stop ovulating as a result.
When a female’s age matures, the number of follicles within the ovaries (which are small poches filled with liquid and also eggs) and the quality of eggs produced decreases. In parallel with this, the risk of a miscarriage and delivering a baby with genetic anomalies, unfortunately increases. The chances of pregnancy decrease when a female is more mature in age.

Can this process be stopped?
Unfortunately, we do not have a chance to freeze time. But we have the chance to freeze the eggs.
Developments in vitro fertilization and in particular laboratory techniques have shown to have successful applications and solutions that are used during egg freezing and thawing. This allows the frozen eggs to successfully survive the thawing process. A pregnancy can then occur at the age of 45 with egg frozen at the age of 35. Moreover, since the egg has a biological age of 35, the chances of pregnancy and a live birth will be higher.
Due to the increasing of women putting emphasis on their career planning and delaying marriage to a later age or having children, the urge for a pregnancy increases with age. Theoretically, there is egg production in the body until menopause, but the chances of becoming pregnant due to age, especially after 42-43 years, are considerably reduced. It is known that the count and quality in eggs accelerates especially around 39-40 years.
When should Egg freezing be considered?
This question can be easily answered and simply yes for all women who have no plan for a child in the near future or who are not sure whether they wish to conceive..
Egg freezing is one way of not to struggle and face the social pressure of not having a child and reduce the level of anxiety in women, egg freezing offers more freedom in planning about life. The thought of that you may be able to conceive with your own eggs at a later age, at any given time and under any condition is quite comforting.
Although social causes are among the most important reasons for freezing eggs, it is especially recommended that the patient freeze their eggs if they have had or have medical conditions. These situations are:

Decrease in egg reserve
Women who have to undergo surgery for problems that are not related to the ovaries but may reduce the egg reserve postoperative (e.g. large chocolate cysts, etc.)
Women who will receive chemotherapy or especially abdominal radiotherapy for any reason;
Women who are expected to enter at an early age, menopause due to having a genetic disorder or premature menopause in their family history.
Are there any tests that should be done before egg freezing?
Some hormone tests are necessary (TSH, AMH, prolactin etc.) and screening for Hepatitis etc. are required before starting treatment to obtain healthy and quality eggs. As well as an antral follicle count scan to monitor the egg reserve.

How long does the treatment process last?
In treatment, follicles containing eggs are targeted and follicle growth is encouraged. To stimulate the follicles, stimulation begins early on in the cycle, i.e. day 2 or 3. Short protocols are used, so hormonal treatment is administered in the form of daily subcutaneous injection to stimulate as many of the antral follicles. An ultrasound examination will be needed at least 3-4 times on average during treatment to monitor follicle growth. The length of the treatment and stimulation is generally between 8-11 days (the days may vary according to the response to the stimulation). At the end of the stimulation, when there are a sufficient number of follicles at a certain size develop, the last trigger injection (to induce ovulation) is administered and the egg collection is performed after 34-36 hours after this.
In other words, the average time from the beginning of the treatment until the egg collection day is 10-14 days.
After the eggs are collected, they are frozen by the embryologist under the microscope, they check to control how many of the eggs are mature (M2) and freeze them accordingly.
Is it sensible to freeze eggs when there is a low egg reserve?
Absolutely. A low egg reserve can indicate that only a small number of eggs can be obtained at one time. In this case, to increase the number of frozen eggs, the collection process can be done more than once to create an egg pool.
PRE-IMPLANTATION GENETIC SCREENING (PGS). WHAT’S GENDER SELECTION?
The purpose of preimplantation genetic screening is to identify whether an embryo carries the correct genetic structure and when an embryo has been cleared as normal, the said embryo can then be transferred to the mother’s uterus. There are two main factors that affect the implantation of the embryo: the embryo and it’s the uterus environment.
An embryo that is genetically healthy is more likely to lead to a viable pregnancy meaning it has a higher chance will attach and go on to a live birth. When In vitro fertilization and genetic testing are combined together, it gives a higher chance to select a healthy embryo. With PGS it can be determined whether there is a numerical or structural problem with the chromosomal structure of an embryo.

Who is preimplantation genetic screening suitable for?
All couples wanting a child can theoretically perform genetic screening of the embryos. However, it is not advised to avoid unnecessary costs of the genetic screening. In cases where it is really necessary is when we would be insistent on the genetic testing. In this context, although there is no scientific consensus in some cases, embryologic genetic screening is generally recommended in the following situations:
- Genetic problems known to one or both partners (if they have abnormal chromosome counts: Turner Syndrome 45, X0, Kleinfelter
- Syndrome 47, XXY, translocation carriers etc.);
- Although spouses have normal genetic structure, there is an increased genetic defect seen within the embryos;
- Repeated negative outcomes after a transfer;
- Couples who suffer with recurrent miscarriages;
- Couples who already have children with genetic problems;
- Couples who require IVF because of the females mature age;
- Couples whose sperm have been found to have an increased genetic problem or whose sperm counts are low.
- Can we give information about the genetic structure of the embryo by the PGS method?
- The genetic screening of the embryo can be used to assess the genetic structure of the embryo to determine whether there are the correct number or any structural problems with the chromosomes. So 46 chromosomes are complete and normal, missing or extra chromosomes, are determined as abnormal.
How is a biopsy carried out from an embryo?
A few cells are removed from the embryo and this is carried out via a laser with the guidance of a microscope by the embryologist. The biopsy of the blastomere (usually taken in the embryo 3 days at the 8-10 cell stage) or trophectoderm (outer cell mass of the embryo at the blastocyst stage) is used for genetic screening. A trophectoderm biopsy is preferred because there is less risk to damaging the embryo and an increased chance of determining which embryo is healthy-unhealthy, as at day 3 there is mozaism in embryo and chance to lead to inaccurate results.
What are the tests used for PGS?
Array CGH (Comparative Genomic Hybridization): The genetic material in the cells are obtained by the trophectoderm biopsy which is performed at the blastocyst stage of the embryo development (embryos are 5-6 days old).

There are 22 pairs of chromosomes in the body cells and the 2 sex chromosomes (X, Y).
NGS (Next Generation Sequencing): Differences from NGS Array CGH are the technical differences in the examination order; other than this, the biopsy time is the same. By this method, all chromosomes are evaluated. The success of detecting mosaic embryos according to the Array method is higher.
(Mosaic embryo: an embryo with both normal and abnormal chromosomal structures)

Can a diagnosis of a known genetic anomaly (mutation) be established with PGS?
PGS is not sufficient for the diagnosis of diseases due to a specific genetic anomaly (e.g. single-gene disorders such as X-linked diseases, Mediterranean anaemia, muscle diseases etc.). Specific and detailed research is required to determine the gene mutation. And before this research, a preconditioning process called set-up is required to determine exactly which gene to evaluate in the genetic makeup. For the set up process, blood is required from both partners and if they have a biological child then them also, a detailed study of the blood is carried over a period of 1-2 months. For rare mutations, the set-up time may take longer. After the set-up is completed, the IVF treatment can only then be started.
What is the difference between Pre-implantation Genetic Diagnosis (PGD) and Pre-implantation Genetic Screening (PGS)?
In the PGD method, except for technical differences, a limited number of chromosomes can be screened. For PGD, minimal chromosomes i.e. up to 5-9 kinds of chromosomes after a 1 or 2 cell at day 3 (biopsy staining (FISH) or PCR method to be taken at embryos that are at 8-10 cell stage. In addition, the PGD method is particularly preferred in the diagnosis of certain single gene disorders.