What Is a Coronary Artery Bypass?
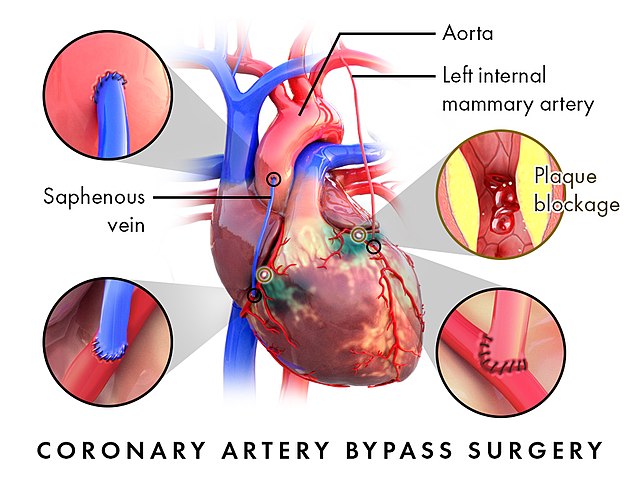
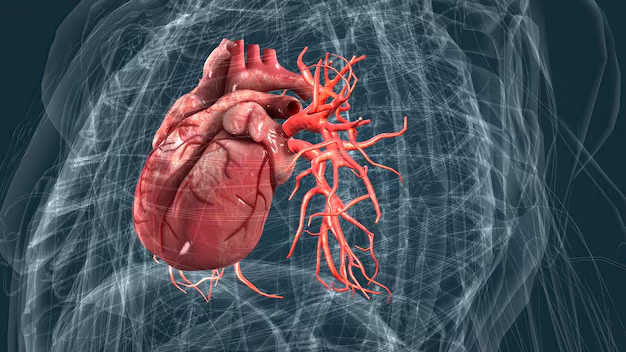
Coronary artery disease is the most common heart disease so that coronary artery bypass graft (CABG) surgery is one of the the most commonly performed cardiac surgery in the world. Coronary arteries supply your heart muscle with oxygen-rich blood. If there is too much plaque (fat and cholesterol) build up in the wall of the arteries, they can be narrowed or even blocked. When the enough blood can not pass through the arteries, heart muscle starves to oxygen and heart attack ocurs. Coronary artery bypass surgery is a surgical option for the patients who can not be treated with angioplasty.
CABG Procedures
In coronary artery bypass surgery, the narrowed or blocked parth of the arteries are bypassed with healthy artery or vein grafts to increase blood flow and supply the heart muscle with oxygen and nutrients. Usually operation takes around 4-5 hours. During the surgery the surgen temporarily stops the heath. The blood circulation in the body will be supplied with the help of a pump machine. It calls on-pump CABG procedure. After surgery when blood start flow in to the heart, the heart starts beating on its own.
For some patients surgeons are not required to stop the heart during the surgery the heart continues to beat on its own this procedure calls off-pump CABG surgery. According to patients heart anatomy and health status our surgeon eill be decided whether to perform the surgery on-pump or off-pump.
Symptoms
Angina, or chest pain and discomfort, is the most common symptom of CAD. Angina can happen when too much plaque builds up inside arteries, causing them to narrow. Narrowed arteries can cause chest pain because they can block blood flow to your heart muscle and the rest of your body.
For many people, the first clue that they have CAD is a heart attack. Symptoms of heart attack include
- Chest pain or discomfort (angina)
- Weakness, light-headedness, nausea (feeling sick to your stomach), or a cold sweat
- Pain or discomfort in the arms or shoulder
- Shortness of breath
Over time, CAD can weaken the heart muscle. This may lead to heart failure, a serious condition where the heart can’t pump blood the way it should.

Risk factors
Overweight, physical inactivity, unhealthy eating, and smoking tobacco are risk factors for CAD. A family history of heart disease also increases your risk for CAD, especially a family history of having heart disease at an early age (50 or younger).
To find out your risk for CAD, your health care team may measure your blood pressure, blood cholesterol, and blood sugar levels.
Conditions that can increase risk
High blood pressure. High blood pressure is a major risk factor for heart disease. It is a medical condition that happens when the pressure of the blood in your arteries and other blood vessels is too high. The high pressure, if not controlled, can affect your heart and other major organs of your body, including your kidneys and brain.
Unhealthy blood cholesterol levels. Cholesterol is a waxy, fat-like substance made by the liver or found in certain foods. Your liver makes enough for your body’s needs, but we often get more cholesterol from the foods we eat.
If we take in more cholesterol than the body can use, the extra cholesterol can build up in the walls of the arteries, including those of the heart. This leads to narrowing of the arteries and can decrease the blood flow to the heart, brain, kidneys, and other parts of the body.
There are two main types of blood cholesterol:
- LDL (low-density lipoprotein) cholesterol, which is considered to be “bad” cholesterol because it can cause plaque buildup in your arteries.
- HDL (high-density lipoprotein) cholesterol, which is considered to be “good” cholesterol because higher levels provide some protection against heart disease.
High blood cholesterol usually has no signs or symptoms. The only way to know whether you have high cholesterol is to get your cholesterol checked. Your health care team can do a simple blood test, called a “lipid profile”.
Symptoms
Diabetes mellitus. Your body needs glucose (sugar) for energy. Insulin is a hormone made in the pancreas that helps move glucose from the food you eat to your body’s cells for energy. If you have diabetes, your body doesn’t make enough insulin, can’t use its own insulin as well as it should, or both.
Diabetes causes sugar to build up in the blood. The risk of death from heart disease for adults with diabetes is higher than for adults who do not have diabetes.2 Talk with your doctor about ways to prevent or manage diabetes and control other risk factors.
Obesity. Obesity is excess body fat. Obesity is linked to higher “bad” cholesterol and triglyceride levels and to lower “good” cholesterol levels. Obesity can lead to high blood pressure and diabetes as well as heart disease. Talk with your health care team about a plan to reduce your weight to a healthy level

Other factors that can increase risk :
Genetics and family history
When members of a family pass traits from one generation to another through genes, that process is called heredity.
Genetic factors likely play some role in high blood pressure, heart disease, and other related conditions. However, it is also likely that people with a family history of heart disease share common environments and other factors that may increase their risk.
The risk for heart disease can increase even more when heredity combines with unhealthy lifestyle choices, such as smoking cigarettes and eating an unhealthy diet.
Age and Sex
Heart disease is the number one killer of both men and women. Heart disease can happen at any age, but the risk goes up as you age.
Race and ethnicity
Heart disease and stroke can affect anyone, but some groups are more likely to have conditions that increase their risk for cardiovascular disease.
Heart disease is the leading cause of death for people of most racial and ethnic groups in the United States, including African Americans, American Indians and Alaska Natives, and White people. For Asian American, Pacific Islander, and Hispanic people, heart disease is second only to cancer.

Treatment and recovery
Cardiac rehabilitation is an important program for anyone recovering from a heart attack, heart failure, or other heart problem that required surgery or medical care. In these people, cardiac rehab can help improve quality of life and can help prevent another cardiac event. Cardiac rehabilitation is a supervised program that includes
- Physical activity
- Education about healthy living, including healthy eating, taking medicine as prescribed, and ways to help you quit smoking
- Counseling to find ways to relieve stress and improve mental health
A team of people may help you through cardiac rehabilitation, including your health care team, exercise and nutrition specialists, physical therapists, and counselors or mental health professionals
Treatment and recovery
If you have CAD, your health care team may suggest the following steps to help lower your risk for heart attack or worsening heart disease:
- Lifestyle changes, such as eating a healthier (lower sodium, lower fat) diet, increasing physical activity, reaching a healthy weight, and quitting smoking
- Medicines to treat risk factors for CAD, such as high cholesterol, high blood pressure, or an irregular heartbeat
- Surgical procedures to help restore blood flow to the heart






