What is a liver transplant?
A liver transplant is a major operation where a diseased liver is removed and replaced by a liver from a donor. It is a life-saving treatment for some patients with cirrhosis and end-stage liver disease (ESLD).
There are three main stages to having a liver transplant:
- Assessment – to find out if you’re able to have a liver transplant
- Going on the waiting list – if suitable, you’ll need to wait for a healthy liver to become available, this may take several months
- Liver transplant surgery – if a liver becomes available, you’ll need to go into a transplant centre for the operation
This is a long and often difficult process. It’s important to understand the benefits and risks of a liver transplant and what life might be like after the operation.


Who can have a liver transplant?
A liver transplant is a possible treatment for patients with end-stage liver disease. To be able to have a liver transplant, the benefits of the operation must outweigh the risks.
The following groups of patients may be suitable for a liver transplant:
- Patients with decompensated cirrhosis (also known as decompensated end-stage liver disease)
- Patients with compensated cirrhosis who go on the develop hepatocellular cancer in the liver
- Patients with sudden, acute liver failure who haven’t had long term liver disease
There are also liver diseases where a liver transplant is offered primarily to improve quality of life. This includes:
- Polycystic liver disease. These patients may require a liver transplant due to liver enlargement and poor quality of life. Associated polycystic kidney disease may require a combined liver and kidney transplant.
- Liver transplants are sometimes offered to patients with symptoms such as severe itch or confusion (encephalopathy) who are not responding to standard treatments
What is end-stage liver disease?
End-stage liver disease is when your liver is damaged beyond repair due to chronic liver disease or acute liver failure. Cirrhosis of the liver happens with long-term liver diseases. Cirrhosis is scarring of the liver. This usually happens after the other stages of damage from conditions that affect the liver.
Diseases that may lead to end-stage liver disease
- Alcohol-related liver disease
- Non-alcoholic fatty liver disease (NAFLD)
- Viral hepatitis (e.g. hepatitis B, hepatitis C)
- Primary biliary cholangitis, sometimes called primary biliary cirrhosis (PBC)
- Primary sclerosing cholangitis (PSC)
- Autoimmune hepatitis (AIH)
- Primary hepatocellular carcinoma (HCC) on a background of chronic liver disease
- Occasionally the cause of end-stage liver disease is unknown
Scarring of the liver
This is known as cirrhosis.
Patients with end-stage liver disease are usually said to have either compensated cirrhosis or decompensated cirrhosis.
Decompensated Cirrhosis
This is also known as decompensated liver disease. Patients with decompensated cirrhosis have more severe symptoms and complications.
Symptoms of decompensated cirrhosis might include:
- Yellow discolouration of the skin (jaundice)
- Fluid retention with abdominal distension (ascites)
- Leg swelling (oedema)
- Confusion (encephalopathy)
- Bleeding from abnormal blood vessels (varices) in the oesophagus and stomach (internal bleeding)
Patients with decompensated cirrhosis are at increased risk of dying from complications of liver disease. Their symptoms can severely affect their quality of life. In these circumstances, liver transplantation can be beneficial.
Compensated Cirrhosis
The liver of patients with compensated cirrhosis still works relatively well, despite the scarring that comes with end-stage liver disease. These patients often have no or few symptoms, but still need to be treated. They are not usually candidates for a liver transplant.
However, sometimes patients with well-compensated cirrhosis can develop hepatocellular cancer (HCC) in their liver. Under certain circumstances they may be offered a liver transplant as a potentially curative treatment, if other treatments are not suitable.
Disadvantages of a liver transplant
A liver transplant has lots of advantages but it also has some disadvantages, which may make it too risky for some patients.
The main disadvantages are:
- A liver transplant is a major operation lasting 5-8 hours
- The surgery can place a strain on your organs
- You have to take powerful immunosuppressant medicines afterwards, which can lead to other serious medical problems.
Reasons why you might not be able to have a liver transplant
Common reasons why a liver transplant may not be the right treatment for you include:

- You are too ill or frail to cope with the surgery and aftercare
- You have recently had cancer, a serious infection, a heart attack or a stroke
- You may struggle taking the immunosuppressant medicines after a liver transplant
- Some patients experience psychological difficulties afterwards
Other treatment options
Sometimes it’s better or safer to have other treatments. These include:
- Improving and tailoring medical treatments and medications
- A transjugular intrahepatic porto-systemic shunt (TIPSS) – this is a tube that lets blood bypass the liver so it can be carried around the body
- Continuing to avoid alcohol (if your liver disease is alcohol-related)
- Nutritional support or exercise programs
Steps towards a liver transplant
If your liver doctor thinks that a liver transplant is a possible treatment option, you will be referred for an assessment at a liver transplant centre. This may be as an inpatient or an outpatient, depending on the centre.
You will be seen and assessed by a consultant transplant anaesthetist. The anaesthetist is the doctor responsible for giving you an anaesthetic and monitoring your condition during the operation. The anaesthetist will review you at either a pre-assessment clinic or during your in-patient assessment stay.
During your assessment you will have lot of medical tests. These are designed to make sure you are physically fit enough to have a liver transplant.
If a suitable liver is offered to you, your transplant team will call to discuss this with you. They may give you some medical information about your donor and discuss potential risks and benefits. If you’re happy to proceed with the possible transplant, you’ll be asked to come to the transplant centre.
We understand that this is a stressful time. Please ask if you would like to bring someone with you to the transplant centre.
How is liver transplant surgery performed?
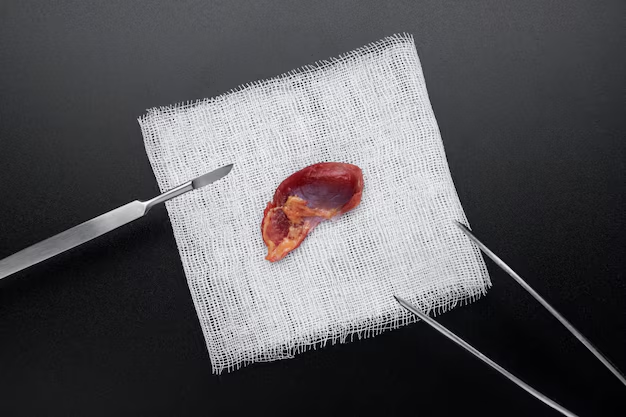
A donor liver is transplanted in the same place as your own liver. This involves the removal of the diseased liver and replacement with the donated liver.
The operation time varies depending on complexity of the procedure. It is often between 5-8 hours.
The medical name for the procedure is an ‘Orthotopic Liver Transplant’. It can be divided into two main stages:
Stage 1: Removal of the Diseased Liver
After you have been put to sleep under anaesthetic, the surgery will begin.
Your damaged liver will be removed and the donor liver will be transplanted into its place.
The incision (cut) used will be in the upper half of your abdomen either shaped like a hockey stick or like an upside-down Y, depending on surgeon choice.
The removal of your own liver can be done in two ways. This depends on what’s best option for you and the personal choice of the surgeon.
- Either by removing the main vein going up to the heart and replacing it with the main vein from the donated liver. The vein is called the inferior vena cava, and this method is known as caval replacement or the classical procedure.
Or,
- By leaving your main vein place and attaching the new liver to it. This is known as a side-to-side cava-cavostomy or the ’piggy-back’ method.
During the removal of your liver the blood vessels into and out of the liver are cut and the bile duct (tube) draining bile from the liver into the small bowel is also cut.
Stage 2: Transplanting The Donated Organ
The donated liver is connected in the following way:
- The blood vessels going into and out of the new liver will be connected to your own blood vessels.
- The gallbladder of the transplanted liver will be removed and the bile duct (the tube carrying bile into the bowel) will be connected to your own bile duct. Usually, this is a direct join between the donor bile duct and your bile duct.
An adult patient may be able to receive a ‘split liver’. This is made up of the right half of the liver and half of the left side (called an ‘extended right lobe’ liver transplant). The smaller left part of the liver is then used for a child patient. This is a more complex operation and the transplant centre will discuss this option with you during the assessment period and at the time it is offered.
For most operations one or two drains are inserted into your abdomen at the end of the operation to drain any fluid or blood that collects around the transplanted liver following the operation. Your skin wound is then closed.
How long will you stay in hospital?
You can expect to be in hospital for 7-14 days after a liver transplant. The first few days are spent in the intensive care unit to allow the extensive monitoring that is required. If you are recovering well from the surgery, the transplant team will be happy for you to be discharged home.
What happens next?
You will only be discharged from hospital when:
- You are physically strong enough
- Your immunosuppressant medication levels are adequate
- You have learnt enough about your condition to look after yourself at home. This will include information about your medications, knowing how to look for symptoms of rejection or infection, and information about any lifestyle changes you need to make.







