What is a knee replacement surgery?
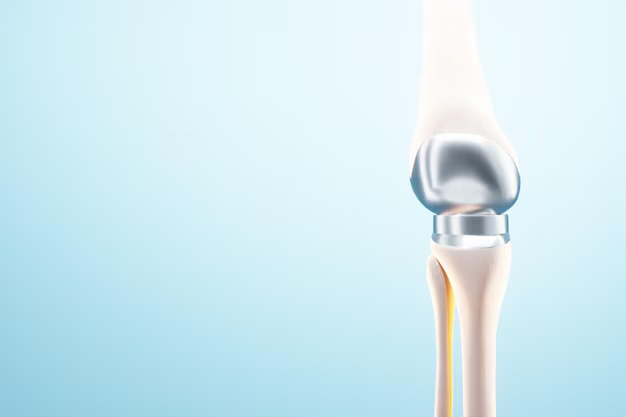
Total knee replacement also known as total knee arthroplasty (TKA) is one of the most common orthopedic surgery treatment in which severely damaged by diseased knee replaced with artificial joint (prosthesis) made of titanium and polyethylene. Depending on the patients health status the prothesis can be fiexed directly to the bone or by using bone cement. Sometimes surgeons use both methods if required.
Total knee replacement usually performs to the adult patients at any age however it is usually performes to patients between 60 to 80 years old. Patients are good candidates for the surgery who are suffering from osteoarthritis, rheumatoid arthritis, posttraumatic arthritis. These diseases can cause destruction of cartilage and damage to the other parts of the knee joint. Such damages leads to severe pain, difficulty with mobility, limit the abilability to sit, stand, walk and carry objects. The goals of the surgery are pain relief, improved function, mobility and quality of life.

Reasons for the procedure
Knee replacement surgery is a treatment for pain and disability in the knee. The most common condition that results in the need for knee replacement surgery is osteoarthritis.
Osteoarthritis is characterized by the breakdown of joint cartilage. Damage to the cartilage and bones limits movement and may cause pain. People with severe degenerative joint disease may be unable to do normal activities that involve bending at the knee, such as walking or climbing stairs, because they are painful. The knee may swell or “give-way” because the joint is not stable.
Other forms of arthritis, such as rheumatoid arthritis and arthritis that results from a knee injury, may also lead to degeneration of the knee joint. In addition, fractures, torn cartilage, and/or torn ligaments may lead to irreversible damage to the knee joint.
Candidates For Beard And Mustache Transplantation
If medical treatments are not satisfactory, knee replacement surgery may be an effective treatment. Some medical treatments for degenerative joint disease may include, but are not limited to, the following:
Anti-inflammatory medications
Glucosamine and chondroitin sulfate
Pain medications
Limiting painful activities
Assistive devices for walking (such as a cane)
Physical therapy

Cortisone injections into the knee joint
Viscosupplementation injections (to add lubrication into the joint to make joint movement less painful)
Weight loss (for obese persons)

Risks of the procedure
As with any surgical procedure, complications can occur. Some possible complications may include, but are not limited to, the following:
Bleeding
Infection
Blood clots in the legs or lungs
Loosening or wearing out of the prosthesis
Fracture
Continued pain or stiffness
The replacement knee joint may become loose, be dislodged, or may not work the way it was intended. The joint may have to be replaced again in the future.
Nerves or blood vessels in the area of surgery may be injured, resulting in weakness or numbness. The joint pain may not be relieved by surgery.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Before the procedure
Your doctor will explain the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure.
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
In addition to a complete medical history, your doctor may perform a complete physical examination to ensure you are in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
Notify your doctor if you are sensitive to or are allergic to any medications, latex, tape, and anesthetic agents (local and general).

Notify your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop these medications prior to the procedure.
If you are pregnant or suspect that you are pregnant, you should notify your doctor.
You will be asked to fast for eight hours before the procedure, generally after midnight.
You may receive a sedative prior to the procedure to help you relax.
You may meet with a physical therapist prior to your surgery to discuss rehabilitation.
During the procedure
Aftercare is essential for the operation to give successful results. After undergoing the beard transplant, during the hair restoration period, the patient should adhere to the following for healthy hair growth:
- Keep their head up.
- Keep the implanted areas away from the water for at least 72 hours after the operation.
- Stop doing hard work or exercise for 15 days since it may cause implanted hair follicles to fall.
- Keep away from sunlight, heat, and high humidity for at least a month.
- Refrain from swimming in the sea for three months and in the pool for two months.
- Avoid smoking for at least two months after the operation because it hinders the growth of transplanted hair follicles.
- Stay away from experiencing the Turkish bath or sauna for a month.
- Plasma needles (PRP) are recommended as they strengthen the implanted follicles.
- Keep taking the necessary treatments and medications your doctor prescribes to recover faster and support beard growth.
- Refrain from sexual intercourse for a week.
- Avoid standing up directly under rain or dust, protecting yourself from damaging the implanted hair follicles.






